In such cases, the indication for AAA craniotomy was decreased risk of general anesthesia in comparison to the possibility of safe resection of small lesions located outside the eloquent areas with the use of a local anesthetic. The majority of patients presented with convexsital/superficially located lesions not exciding 3 cm. There were 98 men and 66 females from 18 to 77 years of age. At this moment, 164 patients were operated with various pathological conditions. The AAA craniotomy protocol was applied in our clinic from 2006. This article represents our experience of using the AAA craniotomy technique in patients with lesional epilepsy. The awake craniotomy with intraoperative neurophysiological monitoring allows improving the results of surgical treatment, to increase the extent of surgical resections at the same time minimizing the neurological complications and reducing the length of hospitalization.ĭespite the modern possibilities of functional magnetic resonance imaging (fMRI), tractography, and intraoperative navigation, only a direct contact with the patient during the intervention allows achieving better functional results. All these methods have their disadvantages and advantages and have been widely reported in literature.
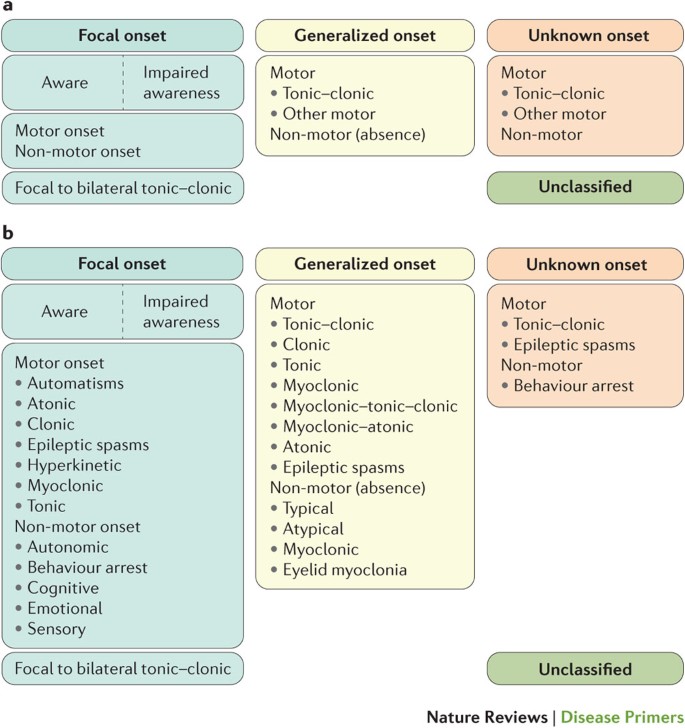
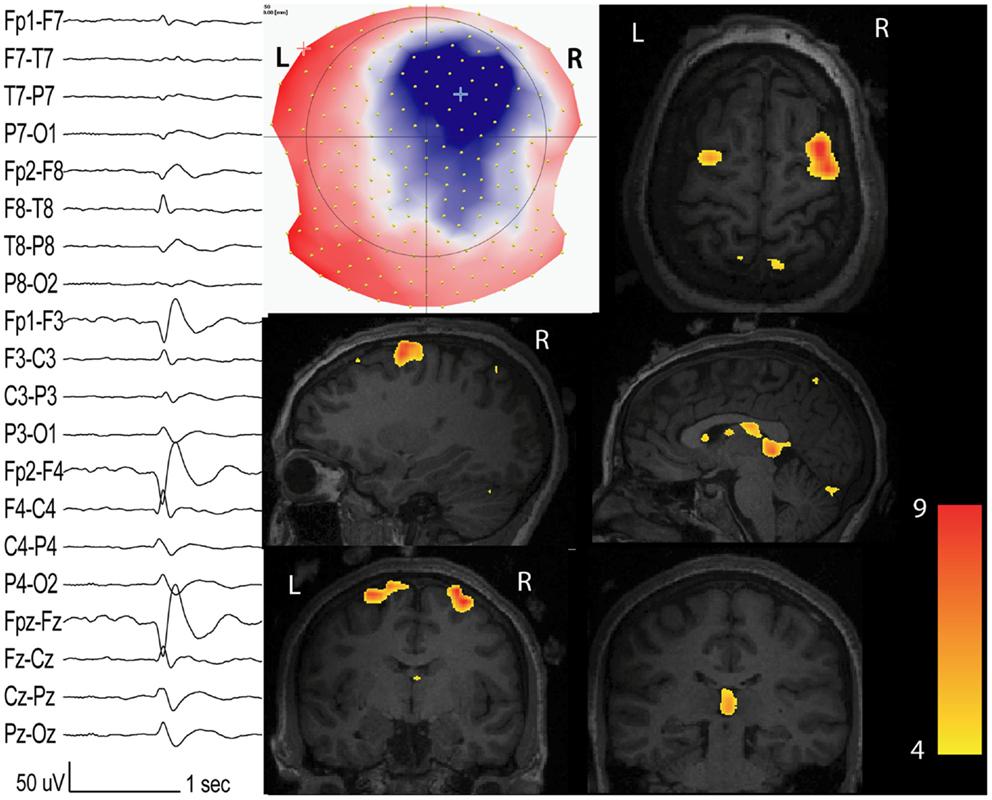
Hansen in 2013 and monitored anesthesia care (MAC). Ingvar in 1950s awake–awake–awake (AAA), suggested by E. The possibilities of intraoperative brain mapping and neurophysiological monitoring, provided by awake craniotomy, allow its implementation even in pediatric patients with mental disorders.Ĭurrently, there are three fundamentally different approaches of performing awake craniotomy: asleep–awake–asleep (SAS) developed and modified by W. Horsley in 1886 and subsequently applied in surgery of convexital tumors, arteriovenous malformations, some superficial aneurysms, and stereotactic neurosurgery. The use of awake craniotomy for the surgical treatment of epilepsy was introduced by V. Keywords: Awake craniotomy, brain mapping, epilepsy, neurophysiological monitoring Excellent seizures control (Engel 1) was achieved in 80% of patients with available catamnesis.Ĭonclusion:Thus, the proposed method allows eliminating the complications associated with sedation and provides radical resection of pathological epileptogenic foci with low complication rate. Minor perioperative complications, including the decrease in blood pressure in six patients and intraoperative convulsions in two patients, were handled and did not led to operation termination or anesthesia conversion. Intraoperative mapping of eloquent cortical areas and subcortical tracts without sedation resulted in total resection of pathological area in 75% of cases with low rate of permanent neurological deficit (two patients). Irrespective of damage location, simple partial and complex partial seizures were seen almost with the same frequency. Results:Most frequently, the pathological foci were located in frontal and parietal lobes nearby eloquent brain areas. Methods:This article describes the results of surgical treatment in 41 patients with various pathologies 31 among them suffered from epilepsy. The aim of this study was to show the advantages of awake craniotomy without sedation, accompanied by intraoperative neurophysiological monitoring in patients with symptomatic epilepsy. Background:The use of awake craniotomy for surgical treatment of epilepsy was applied in surgery of convexital tumors, arteriovenous malformations, some superficial aneurysms, and stereotactic neurosurgery.

 0 kommentar(er)
0 kommentar(er)
